NDIS Infection Prevention and Control Plan
NDIS Infection Control guide: Protect participants & staff, meet compliance, and manage infection risks in all service settings.

Infection prevention and control is a fundamental responsibility for all NDIS providers. Participants often include people with disability who may be more vulnerable to infection due to underlying health conditions, personal care needs, or shared support environments. Without robust infection control systems, providers risk serious harm to participants, workforce exposure, service disruptions, and non-compliance with NDIS Practice Standards.
An effective Infection Prevention and Control (IPC) Plan is not just a policy requirement - it is a critical risk management tool that supports safe, consistent, and high-quality service delivery across all NDIS settings.
This guide explains what an NDIS Infection Prevention and Control Plan is, why it matters, what it must include, and how providers can meet regulatory expectations.
What Is an NDIS Infection Prevention and Control Plan?
An Infection Prevention and Control Plan is a documented framework that outlines how an NDIS provider identifies, prevents, manages, and responds to infection risks across its services. It establishes clear systems, responsibilities, and procedures to minimise the spread of infectious diseases among participants, workers, and others.
Unlike basic hygiene instructions, an IPC Plan:
- Is risk-based and tailored to the provider’s services
- Covers prevention, response, and recovery
- Is supported by training, records, and monitoring
- Is reviewed and updated regularly
All NDIS providers - regardless of size or service type are expected to have infection control systems that are proportionate to their risks.
Why Is an Infection Prevention and Control Plan Critical?
A well-designed Infection Prevention and Control (IPC) Plan is a cornerstone of safe and compliant NDIS service delivery. It provides a structured, proactive approach to identifying and managing infection risks before they escalate into serious incidents.
An effective IPC Plan helps providers to:
- Prevent the spread of infectious diseases by implementing consistent hygiene, cleaning, and risk control measures across all service settings.
- Protect vulnerable participants and workers, particularly where supports involve close personal contact or participants have complex health needs.
- Maintain continuity of essential supports by reducing workforce shortages, service disruptions, and unplanned shutdowns during outbreaks.
- Meet duty of care and Work Health and Safety (WHS) obligations, ensuring providers take reasonably practicable steps to protect both participants and employees.
- Reduce regulatory, legal, and reputational risk by demonstrating compliance with the NDIS Practice Standards and effective risk management systems.
Where infection control systems are weak or poorly implemented, providers face increased risks of reportable incidents, audit non-conformities, service restrictions, enforcement action by the NDIS Commission, and loss of confidence from participants, families, and stakeholders.
Regulatory Framework and Compliance Obligations
Infection prevention and control isn’t just about hygiene - it’s a critical part of delivering safe, high-quality NDIS supports while meeting regulatory requirements. Providers need to have clear systems in place to protect participants, staff, and visitors, while demonstrating compliance with the NDIS framework and national guidance.
1. NDIS Practice Standards (Core Module)
The NDIS Practice Standards set the baseline for safe service delivery. Infection control responsibilities are embedded across several areas to ensure providers manage risks effectively, including:
- Risk Management - identifying and controlling potential infection risks.
- Provision of Supports - delivering services safely.
- Human Resource Management - ensuring staff are trained and competent.
- Incident Management - responding effectively to infection-related events.
Providers must show that they have assessed infection risks and put appropriate controls in place to protect participants and workers.
2. NDIS Quality and Safeguards Commission
The NDIS Quality and Safeguards Commission oversees provider compliance and expects clear, effective infection control systems. Key requirements include:
- Maintaining documented infection control procedures.
- Training staff in infection prevention practices.
- Responding promptly and appropriately to infectious incidents.
- Keeping records that demonstrate compliance.
IPC systems are routinely reviewed during certification audits, verification audits, and incident investigations, so robust documentation and practices are essential.
3. Alignment with National Guidelines
Providers are also expected to align their infection prevention practices with broader public health guidance to ensure safety and consistency. This includes:
- Australian Guidelines for the Prevention and Control of Infection in Healthcare.
- Public health directions issued by state and territory authorities.
By following these frameworks, providers can confidently deliver safe, compliant, and high-quality supports while reducing infection risks for participants and staff.
Core Components of an NDIS Infection Prevention and Control Plan
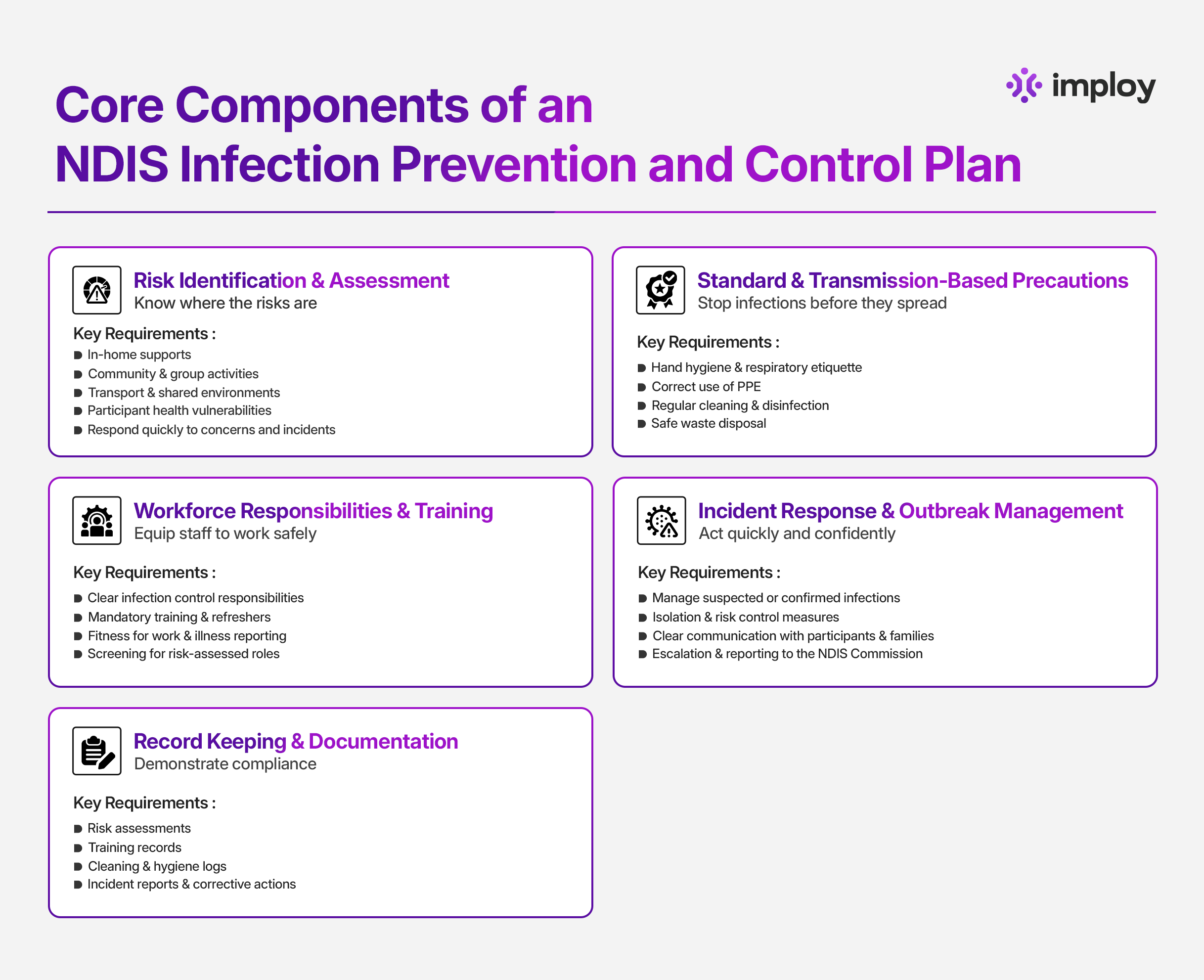
An effective Infection Prevention and Control (IPC) Plan goes beyond written procedures. It A strong Infection Prevention and Control (IPC) Plan goes beyond policies on paper - it sets out clear, practical steps to keep participants, staff, and the wider community safe. Here are the core components every effective IPC Plan should include:
1. Risk Identification and Assessment
The first step in preventing infections is understanding where they might occur. Risk assessments allow providers to identify and manage potential hazards in real-world service delivery.
Key actions include:
- Identifying infection risks across all service types, including in-home supports, community programs, group activities, and transport.
- Considering participant vulnerabilities, such as health conditions or mobility limitations.
- Assessing operational risks, like shared equipment or frequent worker movement.
- Using these insights to implement targeted, practical controls.
2. Standard and Transmission-Based Precautions
Daily precautions are the frontline defence against infection. Clear rules and consistent practices protect both participants and staff.
Key actions include:
- Hand hygiene and respiratory etiquette: proper handwashing, use of sanitiser, and cough/sneeze protocols.
- Personal Protective Equipment (PPE): guidance on when to use it, proper application, storage, and disposal.
- Cleaning, disinfection, and waste management: defined schedules, assigned responsibilities, approved products, and safe disposal practices.
3. Workforce Responsibilities and Training
Staff are central to effective infection control. Clear expectations and training ensure they act safely, confidently, and in line with regulatory requirements.
Key actions include:
- Clearly defining staff responsibilities for infection prevention in day-to-day operations.
- Providing mandatory infection control training with regular refreshers.
- Establishing procedures for reporting illness and assessing fitness for work.
- Screening staff in risk-assessed roles and ensuring ongoing compliance with safety standards.
4. Incident Response and Outbreak Management
Even with strong preventative measures, infections can occur. Preparedness ensures timely, coordinated action to reduce impact.
Key actions include:
- Following procedures for suspected or confirmed infectious cases.
- Implementing isolation and risk mitigation strategies.
- Communicating clearly with participants, families, and staff.
- Escalating concerns to management and health authorities where necessary.
- Reporting to the NDIS Quality and Safeguards Commission as required.
5. Record Keeping and Documentation
Accurate documentation is essential for compliance, continuous improvement, and audit readiness.
Key actions include:
- Maintaining risk assessments, training records, and cleaning/hygiene logs.
- Documenting incidents, outbreaks, and corrective actions taken.
- Regularly reviewing and updating records to ensure practices remain effective and compliant.
Effective infection prevention and control is essential for keeping NDIS participants and staff safe. A well-planned IPC strategy - from risk assessment and precautions to staff training and incident management protects everyone, ensures compliance, and helps services run smoothly. By staying proactive, providers can deliver safe, high-quality support with confidence.
Infection Control Across Different NDIS Service Settings
NDIS providers operate across a range of service environments, each with unique infection risks. Infection Prevention and Control (IPC) measures must be tailored to the setting to remain practical, effective, and compliant.
1. In-Home Supports
In-home services involve entering multiple private households, which increases the risk of cross-contamination. Infection control measures should focus on safe transitions between homes while respecting participant choice and comfort.
- Managing cross-contamination between households
- Practising hand hygiene before and after each visit
- Using PPE where required based on risk
- Cleaning and disinfecting shared equipment between visits
- Balancing safety requirements with respect for the participant’s home environment
2. Community and Group Settings
Community activities and group programs involve shared spaces and higher levels of interaction, increasing exposure risks. IPC measures must support safe participation while remaining flexible.
- Managing infection risks in shared spaces and group activities
- Implementing regular cleaning of commonly touched surfaces
- Monitoring and responding to increased exposure risks
- Communicating clearly with participants and families during outbreaks
- Adjusting activities or group sizes when required
3. High-Risk Supports
Some supports involve close personal contact or participants with higher health vulnerabilities, requiring enhanced infection control measures.
- Managing risks during personal care and close contact supports
- Supporting participants with compromised immunity or complex health needs
- Using additional PPE or hygiene measures where required
- Coordinating infection control practices with healthcare professionals
Overall, IPC Plans should reflect the realities of service delivery and be reviewed regularly to remain effective across all NDIS service settings.
Participant Rights and Communication
Infection prevention and control measures must always be applied in a way that respects participant rights, dignity, and choice. While safety is critical, it should never come at the expense of informed decision-making or person-centred care.
Providers should:
- Communicate infection risks clearly and respectfully, using language that participants can easily understand
- Support informed choice and consent, explaining why specific infection control measures are needed and how they will be applied
- Ensure measures are proportionate, avoiding unnecessary restrictions on participants’ independence, routines, or access to supports
- Provide accessible information, tailored to individual communication needs, cultural considerations, and cognitive abilities
Participants should feel informed and reassured, not confused or excluded. When people understand how infection control measures protect their safety and wellbeing, they are more likely to feel confident, respected, and engaged in their own care.
Common Gaps Identified During NDIS Audits
NDIS auditors frequently identify weaknesses in infection prevention and control systems, particularly where plans exist on paper but are not embedded into day-to-day practice.
Common gaps include:
- Generic or copied IPC plans that are not tailored to the provider’s actual services, settings, or risk profile
- Lack of evidence of staff training, including missing records or outdated training that does not reflect current guidance
- Poor incident documentation, with unclear timelines, incomplete records, or limited follow-up actions
- Plans that do not reflect real service delivery, such as in-home supports, group programs, or high-risk personal care
- Outdated references to public health guidance, indicating plans have not been reviewed or updated regularly
These gaps can result in audit non-conformities, corrective actions, and increased regulatory scrutiny. Addressing them proactively helps providers demonstrate compliance, reduce risk, and strengthen confidence in their infection control systems.
How Imploy Helps?
Imploy is a purpose‑built operations and compliance platform for NDIS and care providers. It supports safer and more efficient service delivery by centralising key administrative, compliance, and workforce functions in a single system.
How Imploy supports infection prevention and control and wider compliance needs:
- Centralised documentation and compliance: Imploy enables providers to store and manage policies, procedures, incident records, and risk assessments in one secure place - helping demonstrate audit‑ready IPC documentation when requested by auditors or commissioning bodies.
- Incident & risk management workflows: Built‑in tools for reporting, tracking, and responding to incidents help record infection‑related events and corrective actions clearly and consistently.
- Workforce training and screening records: Providers can track staff compliance requirements such as training expiry dates, worker screening checks, and qualifications, which are essential for maintaining IPC competence across the workforce.
- Mobile workforce tools: The Imploy mobile app allows support workers to access schedules, record progress notes, and submit incident details in real time, supporting accurate and up‑to‑date data capture as part of infection prevention practices.
- Operational efficiency: By reducing administrative burden through automated rostering, payroll integration, and PRODA claims, providers can focus more on quality care delivery rather than paperwork - including the implementation of IPC procedures.
Imploy’s platform is designed to help providers stay compliant with the NDIS Practice Standards and relevant reporting obligations, while also streamlining everyday operations across care settings.
Final Thoughts
Infection prevention and control is essential for safe, high-quality NDIS services. A well-designed IPC Plan goes beyond paperwork - it actively protects participants, staff, and the community while ensuring compliance.
Providers with a practical, risk-based, and regularly reviewed IPC system can:
- Prevent the spread of infections across service settings.
- Protect vulnerable participants and staff.
- Maintain continuity of supports during outbreaks.
- Demonstrate compliance with NDIS standards and public health guidance.
- Reduce legal, reputational, and operational risks.
By embedding IPC practices into daily operations and using tools like Imploy for documentation, training, and incident management, providers can deliver safe, person-centred care with confidence.
FAQs
1. Do all NDIS providers need an IPC Plan?
Yes. All NDIS providers must have a documented Infection Prevention and Control Plan, scaled to the size, service type, and risk profile of their organisation.
2. How often should an IPC Plan be reviewed?
IPC Plans should be reviewed regularly - at least annually, and updated whenever there are changes in service delivery, staff, participant needs, or public health guidance.
3. How can providers ensure staff follow IPC procedures?
Providers must provide mandatory infection control training, regular refreshers, clearly assign responsibilities, and implement monitoring and supervision systems.
4. Are worker screening checks necessary for infection control?
Yes. Risk-assessed roles require NDIS Worker Screening Checks to help ensure staff suitability for supporting vulnerable participants.
5. How can Imploy help with compliance?
Imploy centralises IPC documentation, training records, incident reporting, and workforce compliance, helping providers stay audit-ready and demonstrate adherence to NDIS Practice Standards.