NDIS Emergency and Disaster Management Plan + Template
A practical guide to NDIS Emergency and Disaster Management Plans, covering compliance requirements, key steps, and downloadable templates.
Emergencies and disasters can happen without warning. For NDIS providers, having a robust Emergency and Disaster Management Plan is not just best practice - it’s a compliance requirement. Such a plan ensures participants are safe, staff know their responsibilities, and providers can respond quickly and effectively.
With tools like Imploy, providers can streamline planning, training, and compliance tracking to meet the NDIS Practice Standards with confidence.
What is an NDIS Emergency and Disaster Management Plan?
An NDIS Emergency and Disaster Management Plan is a structured framework that guides providers on how to prepare for, respond to, and recover from emergencies or disasters. It ensures participants’ safety, supports continuity of care, and helps providers meet NDIS Practice Standards by addressing risks, assigning responsibilities, and outlining clear procedures for any critical situation.
It aligns with NDIS Practice Standards under the Core Module and Governance & Operational Management, ensuring your organisation meets regulatory requirements.
Types of emergencies relevant to NDIS providers include:
- Natural disasters (floods, fires, storms)
- Medical emergencies
- Pandemics or infectious disease outbreaks
- Cybersecurity incidents
- Infrastructure failures (power outages, water supply disruptions)
Why an NDIS Emergency and Disaster Management Plan is Crucial?
Emergencies and disasters can happen without warning. For NDIS providers, having a clear Emergency and Disaster Management Plan is essential to keep participants safe, guide staff, and ensure services continue effectively.
- Ensures Participant Safety - Protects participants during emergencies by providing structured guidance.
- Supports Staff Confidence - Clearly defines roles and responsibilities so staff can act quickly and effectively.
- Maintains Continuity of Care - Helps services continue operating smoothly even during unexpected events.
- Demonstrates Compliance - Meets NDIS Practice Standards and regulatory requirements.
- Minimises Risk - Reduces potential harm to participants, staff, and organisational operations.
A strong plan not only safeguards participants and staff but also demonstrates compliance with NDIS Practice Standards, building confidence and resilience within your organisation.
Key Components of an Effective Plan
A strong NDIS Emergency and Disaster Management Plan is practical, participant-focused, and easy to follow during high-pressure situations. It should clearly outline how risks are managed, how staff respond, and how participant safety is maintained before, during, and after an emergency.
A strong plan includes:
- Risk Assessment - Identify hazards that could affect participants or staff, such as medical emergencies, natural disasters, or operational failures.
- Emergency Procedures - Provide step-by-step actions for each scenario to ensure staff respond quickly and consistently.
- Roles and Responsibilities - Assign clear primary and backup duties so every task is covered during an emergency.
- Communication Plan - Outline who to contact and how, including staff, families, carers, and emergency services.
- Evacuation and Shelter Strategies - Define safe exit routes and temporary shelter options, considering participants’ needs.
- Training and Awareness - Regularly train staff and participants so everyone knows what to do under pressure.
- Review and Testing - Conduct drills and update the plan based on lessons learned to keep it effective and compliant.
Steps to Develop Your Plan
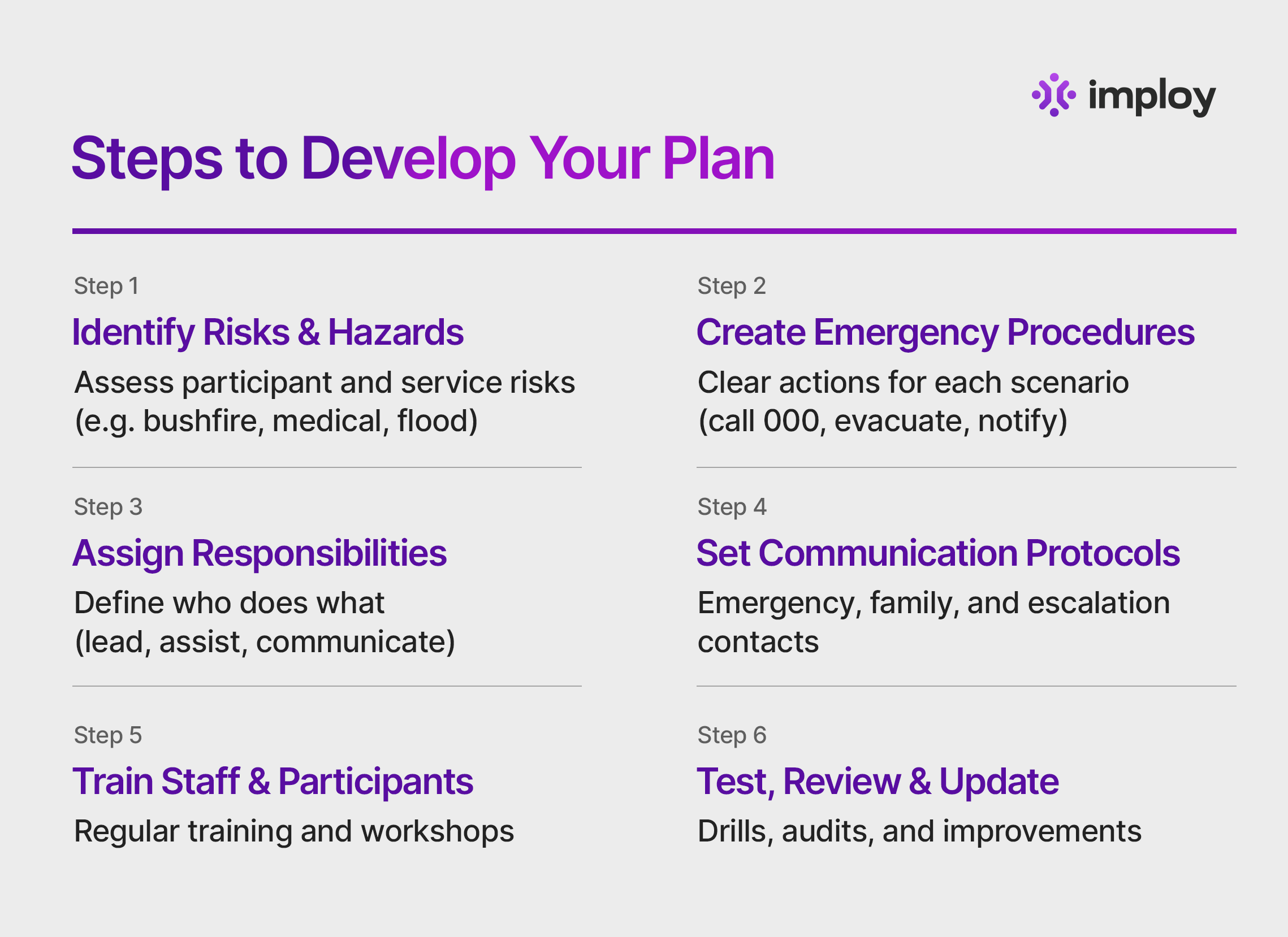
Developing an NDIS Emergency and Disaster Management Plan requires a structured, proactive approach.
By following these six practical steps, providers can reduce risk, protect participants and staff, and ensure compliance with the NDIS Practice Standards while remaining prepared for unexpected events.
Step 1: Identify Risks and Hazards
Begin by assessing the specific risks that may impact your participants, staff, and service delivery. Consider environmental, medical, operational, and technological risks, taking into account where supports are delivered and the individual needs of participants.
Example: If participants live in bushfire-prone areas, fire evacuation and relocation procedures must be included.
Step 2: Create Detailed Procedures
For each identified emergency, document clear, step-by-step procedures that staff can easily follow under pressure. Procedures should be practical, easy to understand, and focused on participant safety and continuity of care.
Example: In a medical emergency, staff should call 000, provide first aid if trained, notify management, and contact the participant’s emergency contacts.
Step 3: Assign Responsibilities
Clearly define who is responsible for each action during an emergency to avoid confusion and delays. Assign primary and backup roles so responsibilities are covered even if key staff are unavailable.Example: One staff member leads evacuation, while another manages communication with families and emergency services.
Example: One staff member leads evacuation, while another manages communication with families and emergency services.
Step 4: Develop Communication Protocols
Establish clear communication pathways for emergencies, including internal escalation and external notifications. Ensure up-to-date contact details are readily accessible for emergency services, families, carers, and key staff.
Effective communication helps maintain coordination, transparency, and participant confidence during critical situations.
Step 5: Train Staff and Participants
Training ensures staff understand their roles and can respond calmly and effectively in emergencies. Regular refresher training, inductions, and participant education help embed emergency preparedness into everyday service delivery. Well-trained teams reduce risk and improve outcomes during real incidents.
Step 6: Test, Review, and Update
Emergency plans must be tested through drills, simulations, and audits to ensure they work in practice. Review and update the plan regularly, especially after incidents, drills, or changes in participant needs or service locations.
Continuous improvement ensures your plan remains relevant, effective, and audit-ready.
A well-developed Emergency and Disaster Management Plan is more than a compliance document - it’s a critical safeguard for participants, staff, and your organisation. By following these steps and regularly reviewing your approach, NDIS providers can build resilience, maintain service continuity, and demonstrate a strong commitment to safety and quality care.
Compliance Requirements
NDIS providers must comply with the NDIS Practice Standards, which include:
- Ensuring participants’ health, safety, and wellbeing
Providers must identify, assess, and manage risks to protect participants at all times. Emergency plans should reflect individual needs such as mobility, communication, and medical requirements. - Maintaining proper documentation
Up-to-date records of emergency plans, staff training, drills, and incidents must be maintained. These documents should be accessible and consistently applied across the organisation for audit purposes. - Meeting governance and operational management obligations
Providers must demonstrate leadership and accountability by assigning responsibilities and regularly reviewing emergency risks. Emergency procedures must be actively embedded into daily service delivery. - Ongoing review and continuous improvement
Emergency plans should be tested and updated regularly, especially after incidents or changes in service delivery. Continuous review ensures the plan remains effective, compliant, and responsive to risk.
How Imploy Helps?
Imploy makes emergency planning simple, compliant, and effective for NDIS providers:
- Ready-to-use Templates: Download NDIS-compliant emergency and disaster management plan templates, saving time and ensuring compliance.
- Automated Compliance Tracking: Track staff training, plan reviews, and incident reports effortlessly.
- Documentation Management: Record drills, incidents, and corrective actions in one secure place.
- Customisable Solutions: Adapt plans for participant-specific needs, locations, and organisational structures.
- Staff Accountability: Assign and monitor roles and responsibilities during emergencies, ensuring everyone knows their duties.
- Notifications & Alerts: Set reminders for plan reviews, training refreshers, and drills so nothing is missed.
- Continuous Improvement Support: Easily update plans based on lessons learned from incidents, drills, or regulatory changes.
With Imploy, managing emergencies is easy, compliant, and always participant-focused.
Final Thoughts
An effective NDIS Emergency and Disaster Management Plan protects participants, staff, and your organisation. Beyond compliance, it builds trust with participants and families, reduces risk, and ensures your team can respond calmly and efficiently when disaster strikes.
With Imploy’s templates and compliance tools, you can create a plan that is practical, participant-focused, and audit-ready - without the stress of starting from scratch.
Frequently Asked Questions (FAQs)
Q1: What is the difference between an emergency plan and a disaster management plan?
An emergency plan focuses on immediate responses to incidents, such as medical emergencies or fires, while a disaster management plan covers preparation, response, and recovery for larger-scale events or prolonged disruptions.
Q2: Who needs to be involved in creating the plan?
All key stakeholders should be involved, including management, support staff, and, where possible, participants and their families. This ensures the plan reflects real participant needs and practical operational procedures.
Q3: How often should the plan be reviewed or updated?
The plan should be reviewed at least annually and updated whenever there are changes to participant needs, service locations, staff, or after an actual incident or drill.
Q4: Are NDIS providers required to train staff in emergency procedures?
Yes. Staff must be trained on their roles and responsibilities during emergencies. Regular refresher training and drills are required to maintain readiness and compliance.
Q5: Can the plan be customised for individual participants?
Absolutely. Each plan should consider participant-specific needs, including mobility, communication, medical conditions, and personal preferences for emergency response.
Q6: What should be done after an emergency or incident occurs?
Conduct a post-incident review to assess what worked, identify gaps, update procedures, and implement improvements. Documenting these steps helps ensure continuous improvement and compliance with NDIS Practice Standards.