How to Stay Compliant as a Support at Home Provider
Stay compliant as a Support at Home provider with clear guidance on safeguarding, staff checks, finances, and quality under the Aged Care Act 2024.

The transition to the Support at Home program represents a significant change in Australia’s aged care system. With stronger safeguards, clearer obligations, and increased regulatory oversight, compliance is now a critical responsibility for all providers.
For Support at Home providers, compliance is not just about meeting legal requirements - it is about delivering safe, high-quality care while protecting older people, staff, and the organisation itself. This blog explains the key compliance obligations and how providers can meet them effectively.
Understanding the Compliance Landscape
Support at Home providers operate within a structured regulatory framework overseen by the Australian Government and the Aged Care Quality and Safety Commission (ACQSC).
1.1 Key legislation and frameworks
Providers must comply with:
- The Aged Care Act 2024The primary legislation for aged care in Australia, establishing participant rights, provider responsibilities, and a focus on safety, quality, and accountability. It also outlines duties under Support at Home and consequences for non-compliance.
- The Aged Care Rules 2025 and transitional arrangements
Provide detailed operational requirements for registration, service delivery, funding, and reporting. Transitional rules guide providers moving from Home Care Packages to Support at Home. - The Aged Care Quality StandardsSet the expected level of care, emphasising dignity, choice, governance, workforce capability, and continuous improvement. Compliance is assessed during audits and reviews.
- The Aged Care Code of ConductDefines ethical expectations for providers, workers, contractors, and volunteers, including integrity, professionalism, and safety. Breaches can lead to regulatory action.
- Privacy and consumer protection legislation
Laws like the Privacy Act 1988 and Australian Consumer Law require secure handling of personal information, transparent pricing, and fair, honest dealings with participants.
1.2 Role of the Regulator
The Aged Care Quality and Safety Commission (ACQSC) is responsible for regulating Support at Home providers and ensuring services are delivered safely and in line with legislative requirements. The Commission monitors compliance through audits, assessments, complaints handling, and ongoing monitoring activities.
Where a provider fails to meet its obligations, the ACQSC has the authority to take regulatory action. This may include issuing compliance notices, placing conditions on a provider’s registration, imposing sanctions, or revoking approval to deliver aged care services. The regulator also works with providers to address risks and drive continuous improvement.
Understanding the role and powers of the ACQSC is essential for providers to operate safely, lawfully, and with confidence under the Support at Home program.
Core Compliance Areas for Support at Home Providers
As a registered Support at Home provider, meeting compliance obligations is central to delivering safe, quality care and operating lawfully under the Aged Care Act 2024 and related legislation. Providers are required to comply with all duties relevant to their registration category, and regulatory action may be taken if requirements are not met.
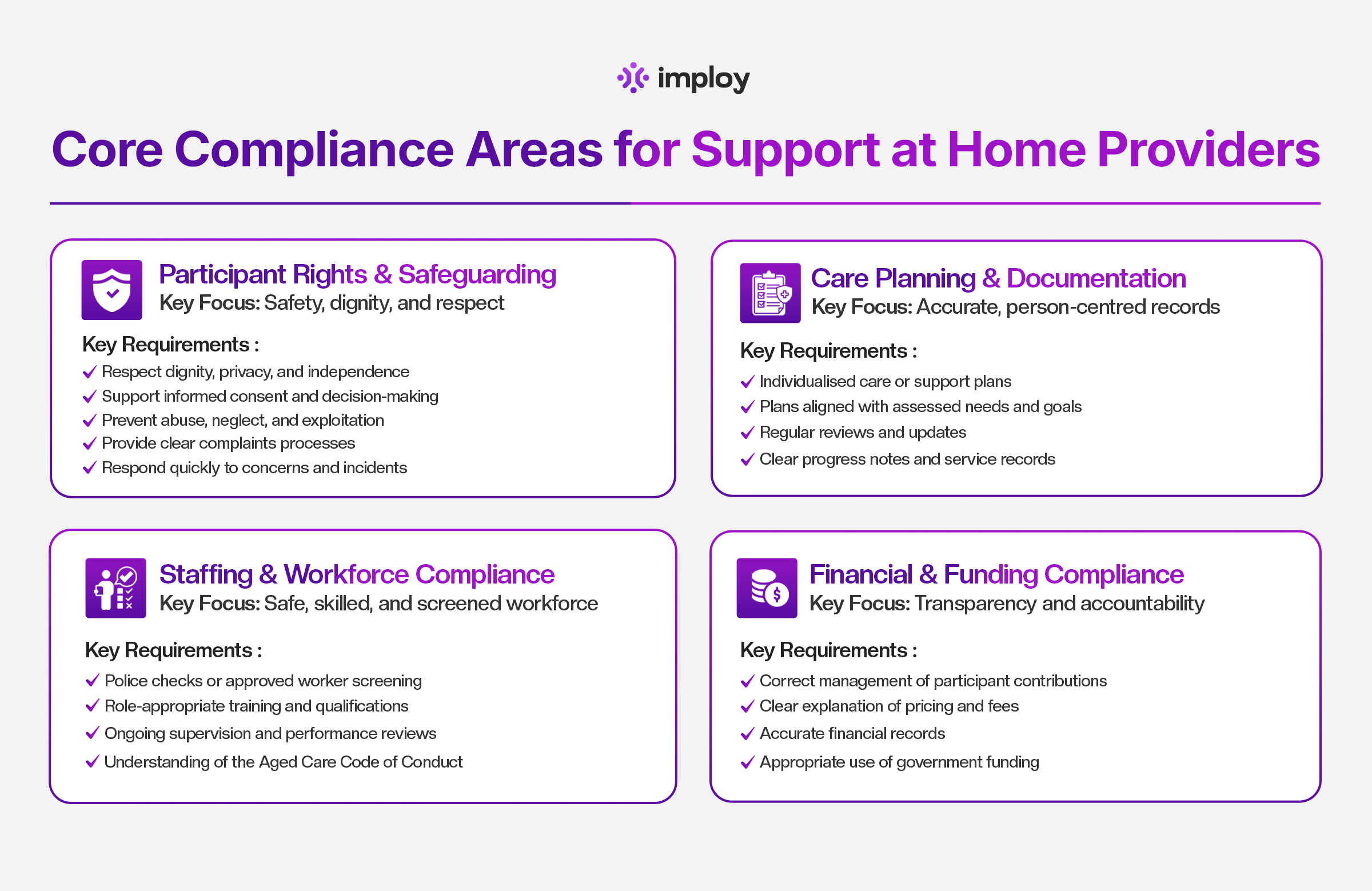
2.1 Participant Rights and Safeguarding
Safeguarding older people is at the heart of Support at Home compliance. Providers must uphold participant rights and ensure their safety, dignity, and wellbeing every day. This includes:
- Respecting participant dignity, privacy and independence.
- Supporting informed consent and decision‑making.
- Protecting participants from abuse, neglect and exploitation.
- Providing clear and accessible mechanisms for feedback and complaints.
- Responding promptly and appropriately to concerns and incidents.
Safeguarding must be integrated into daily service delivery and not treated as a standalone administrative task.
These requirements are part of the core regulatory expectations under the Aged Care Act and Code of Conduct.
2.2 Care Planning and Documentation
Accurate and timely documentation is essential for both compliance and quality care outcomes. Providers should ensure that:
- Individualised care or support plans document participant needs, preferences and goals.
- Care plans are updated regularly and whenever a participant’s circumstances change.
- Progress notes, service records and decisions are clearly and consistently recorded.
- Records support evidence of effective care and service delivery.
Incomplete or poor‑quality documentation is one of the most common compliance issues identified by regulators.
2.3 Staffing and Workforce Compliance
Providers must ensure that their workforce, including employees, responsible persons, contractors and volunteers, meets suitability and screening requirements. Key obligations include:
- Worker screening: All aged care workers and responsible persons must hold a valid police certificate (no older than three years) without disqualifying findings, or a valid NDIS check if they also work in the NDIS sector.
- Providing appropriate training, supervision and performance support.
- Ensuring all workers understand and comply with the Aged Care Code of Conduct.
- Maintaining records of screening, qualifications and ongoing training.
From 2026, new worker screening processes aligned with the NDIS framework will be introduced, further strengthening workforce compliance standards.
2.4 Financial and Funding Compliance
Support at Home places a strong emphasis on financial transparency and accountability. Providers must:
- Manage participant contributions fairly and in line with program rules.
- Communicate pricing and fees clearly and transparently to participants.
- Maintain accurate financial records that reflect funding use and transactions.
- Use government funding appropriately to deliver agreed services and supports.
Providers are required to submit regular financial reports and demonstrate prudent financial management. Failure to meet financial reporting and accountability obligations is a common cause of compliance action.
By understanding and actively managing these core compliance areas, Support at Home providers can ensure they meet regulatory expectations and deliver high‑quality, safe services to older Australians.
Implementing Effective Policies and Procedures
Strong policies and procedures are the foundation of compliance for Support at Home providers. They provide guidance to staff, ensure consistent service delivery, and demonstrate adherence to legislative and regulatory requirements. Well-documented policies also help organisations manage risks, protect participants, and prepare for audits or inspections.
3.1 Required Policies
Support at Home providers should maintain clear, documented policies covering key operational areas, including:
- Incident management and reporting: Procedures for identifying, responding to, documenting, and escalating incidents, including serious incidents under the SIRS framework.
- Infection prevention and control: Measures to minimise infection risks and promote safe hygiene practices for staff and participants.
- Medication management: Safe handling, administration, storage, and recording of medications in accordance with regulatory guidance.
- Emergency and business continuity: Plans to ensure services can continue during emergencies, disasters, or unforeseen disruptions.
- Complaints handling: Processes for receiving, addressing, and resolving participant or family complaints in a timely and transparent manner.
- Privacy and data protection: Guidelines for collecting, storing, and sharing participant information securely, in compliance with privacy laws.
Having these policies in place ensures that staff have clear instructions and that participant care is consistent, safe, and legally compliant.
3.2 Policy Management
Effective policy management goes beyond documentation. Providers should ensure that policies are:
- Aligned with current legislation and regulations: Policies must reflect the latest requirements under the Aged Care Act 2024, Aged Care Rules 2025, and relevant quality standards.
- Reviewed regularly: Policies should be evaluated at least annually or whenever legislative or operational changes occur.
- Clearly communicated to staff: All staff should understand their responsibilities, know where policies are stored, and how to apply them in daily practice.
- Supported by training and supervision: Staff training and ongoing supervision are essential to ensure policies are implemented correctly and consistently.
Crucially, policies must not exist on paper only. Providers should be able to demonstrate in practice that policies are actively followed, monitored, and updated as required. Embedding policies into everyday operations helps mitigate risks, improves participant outcomes, and strengthens organisational accountability.
Risk Management and Quality Assurance
Effective risk management and quality assurance are critical components of compliance for Support at Home providers. They help organisations prevent harm, protect participants and staff, and ensure services meet legislative and regulatory requirements. By embedding risk management and continuous improvement into daily operations, providers can demonstrate a proactive approach to safety, governance, and service quality.
4.1 Identifying and Managing Risk
Providers should actively identify, assess, and manage risks across all areas of service delivery. Key risk areas include:
- Clinical risks: Issues that could directly affect participant health, such as falls, medication errors, or deterioration in health status. Providers should implement care plans, monitoring systems, and staff training to minimise these risks.
- Operational risks: Risks to service continuity, including staffing shortages, equipment failures, or disruptions to service delivery. Contingency plans, flexible rostering, and robust communication protocols can mitigate these risks.
- Financial and governance risks: Risks associated with mismanagement of funding, financial instability, or inadequate organisational oversight. Strong governance, accurate record-keeping, and regular financial reporting help address these risks.
- Compliance risks: Risks arising from failing to meet regulatory obligations, such as reporting, documentation, or policy adherence. Regular compliance audits, staff training, and documented procedures reduce these risks.
Providers should maintain a risk register and develop risk mitigation strategies. Regular reviews ensure that new risks are identified and managed promptly, and that controls remain effective.
4.2 Continuous Quality Improvement
Quality improvement is an ongoing process that strengthens service delivery and compliance. Providers should implement structured activities, including:
- Internal audits: Regular reviews of care delivery, documentation, policies, and procedures to identify gaps or areas for improvement.
- Incident trend analysis: Monitoring and analysing incidents, complaints, and near-misses to prevent recurrence and improve practices.
- Participant feedback: Collecting and acting on feedback from participants and families to enhance satisfaction and service quality.
- Corrective action plans: Implementing targeted strategies to address identified issues and tracking their effectiveness over time.
A strong culture of quality improvement encourages staff to take ownership of compliance, fosters transparency, and ensures services continuously meet participant needs and regulatory expectations.
By combining proactive risk management with ongoing quality improvement, Support at Home providers can demonstrate accountability, reduce harm, and maintain regulatory compliance.
Record Keeping and Reporting
Accurate record keeping and timely reporting are essential for maintaining compliance under the Support at Home program. They help providers demonstrate accountability, support participant safety, and meet regulatory obligations.
5.1 Documentation Standards
Providers must maintain secure, accurate, and up-to-date records covering all aspects of service delivery, including:
- Participant care: Detailed records of assessments, support plans, service delivery, progress notes, and any changes in needs.
- Incidents and complaints: Documentation of all incidents, complaints, investigations, and follow-up actions. This is crucial for identifying trends and mitigating future risks.
- Staff screening and training: Records of police checks, worker screenings, qualifications, training completion, and ongoing competency assessments.
- Financial transactions: Documentation of participant contributions, invoicing, funding allocations, and expenditure.
Records must not only be maintained accurately but also readily accessible for review by regulators or auditors. Providers must follow legal requirements for record retention and data protection to ensure privacy and confidentiality.
5.2 Mandatory Government Reporting
Support at Home providers have specific reporting obligations to demonstrate financial and operational compliance:
- Quarterly Financial Reports (QFRs): Submitted four times a year to show financial viability and the appropriate use of government funding.
- Aged Care Financial Reports (ACFRs): Annual reporting on income, expenditure, assets, and financial performance.
- Provider Operations Collection data: Information on governance, complaints, incidents, workforce, and quality improvement activities.
Timely and accurate reporting is essential. Late, incomplete, or incorrect submissions are a common reason for compliance breaches and may trigger regulatory action. Using digital systems or automated tools can help streamline reporting, reduce errors, and ensure deadlines are met.
Staying Updated with Regulatory Changes
The Support at Home program is continually evolving, with new rules, guidance, and reforms introduced over time. Staying informed is essential for providers to maintain compliance, adapt services, and ensure high-quality care for participants.
Providers should:
- Monitor government and ACQSC updates
- Subscribe to official communications
- Engage with industry associations
- Regularly review policies and training materials
Staying informed reduces compliance risk.
How Imploy Supports Compliance for Support at Home Providers
Managing compliance under the Support at Home program can be complex, but Imploy provides digital solutions to simplify obligations and help providers maintain safety, accountability, and transparency.
1 Workforce Management
- Tracks staff qualifications, training, and competencies.
- Maintains police check and worker screening records.
- Sends automated reminders for expiry or re-certification.
2 Incident and Risk Management
- Enables logging and tracking of incidents in real time.
- Provides analytics to identify trends and improve service quality.
3 Documentation and Reporting
- Maintains secure and accurate participant care records.
- Simplifies submission of financial and operational reports.
- Ensures all documentation is audit-ready and compliant.
4 Policy and Procedure Oversight
- Provides templates and tracking tools for policies and procedures.
- Supports staff training and ensures policies are followed in practice.
- Enables monitoring of compliance across all operational areas.
By centralising compliance tasks, Imploy reduces administrative burden, minimises errors, and allows providers to focus on delivering high-quality, safe care while staying fully aligned with Support at Home requirements.
Final Thoughts
Compliance under the Support at Home program is an ongoing responsibility that affects every part of a provider’s operations. By understanding regulatory expectations, investing in strong governance, and supporting staff with clear systems and training, providers can confidently meet their obligations.
A proactive compliance approach not only reduces risk - it strengthens service quality, builds trust with participants, and supports long-term sustainability.
Frequently Asked Questions (FAQs)
1. What does compliance mean under the Support at Home program?
Compliance under Support at Home means meeting all legal, regulatory, and quality obligations set out in the Aged Care Act 2024, Aged Care Rules 2025, and the Aged Care Quality Standards. It includes safeguarding participant rights, maintaining accurate records, ensuring workforce suitability, managing funding correctly, and cooperating with regulatory oversight.
2. Who regulates Support at Home providers?
Support at Home providers are regulated by the Aged Care Quality and Safety Commission (ACQSC). The Commission monitors compliance through audits, assessments, complaints handling, and ongoing monitoring, and can take enforcement action where obligations are not met.
3. What are the most common compliance risks for providers?
Common compliance risks include poor or incomplete documentation, inadequate safeguarding practices, expired worker screening or training, unclear pricing and financial records, and late or inaccurate government reporting.
4. What safeguarding responsibilities do providers have?
Providers must protect participants from abuse, neglect, and exploitation, uphold dignity and choice, support informed consent, and respond promptly to incidents and complaints. Safeguarding must be embedded into everyday service delivery, not treated as a separate task.
5. How important is documentation for compliance?
Documentation is critical. Providers must maintain accurate, timely, and secure records of care plans, service delivery, incidents, complaints, workforce screening, training, and financial transactions. Poor documentation is one of the most frequent issues identified during audits.





