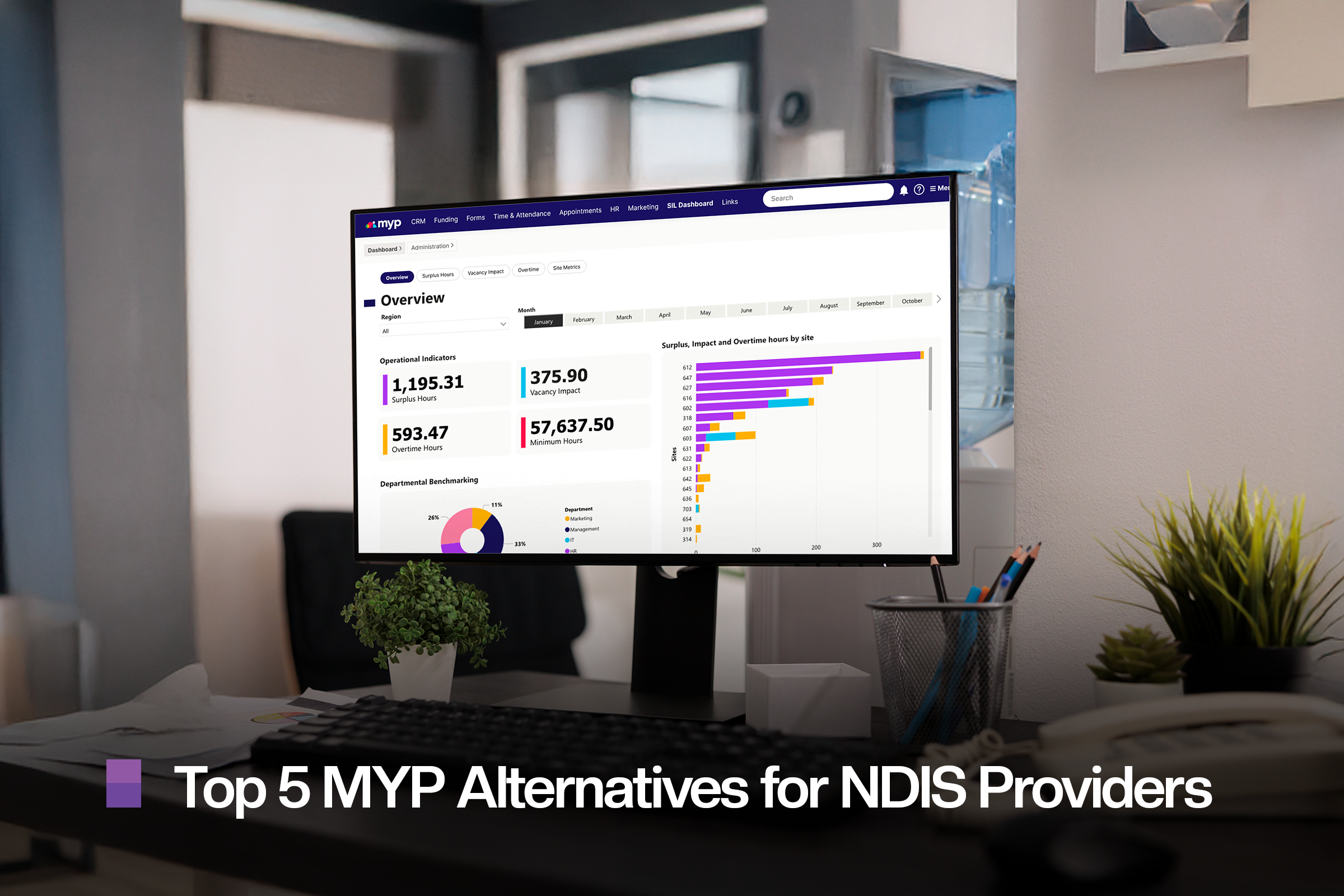
NDIS Restrictive Practices Reporting: What Providers Must Know
NDIS restrictive practices reporting guide: provider obligations, reporting steps, and compliance explained.
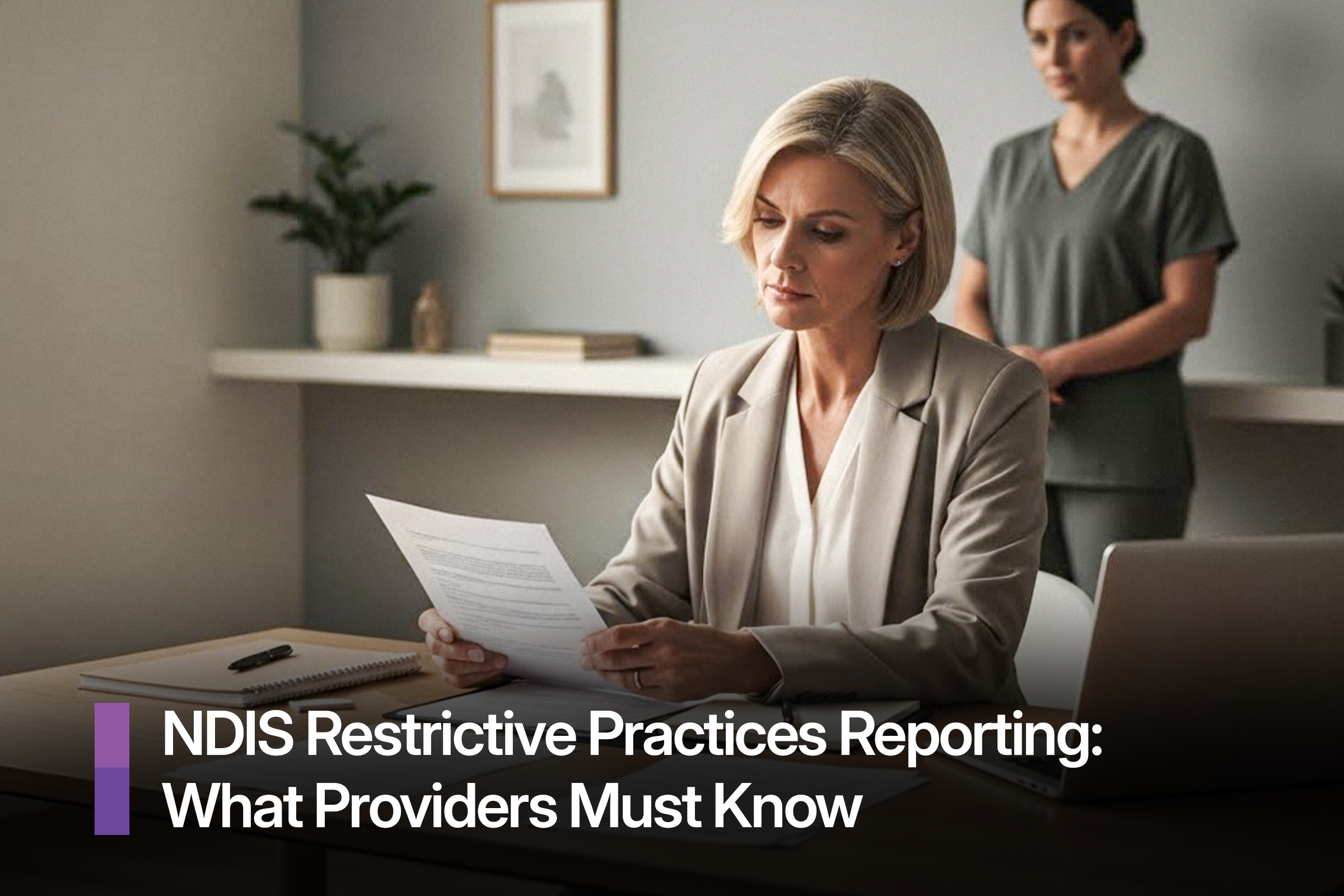
Restrictive practices are one of the most sensitive and closely regulated areas of the NDIS. They directly affect a participant’s safety, rights, and dignity, which is why providers must approach them with care, clarity, and accountability. Understanding when restrictive practices can be used and, just as importantly, how and when they must be reported - isn’t optional. It’s a core legal responsibility overseen by the NDIS Quality and Safeguards Commission.
With more than one million unauthorised restrictive practices reported in a single year, the message from the Commission is clear. Accurate reporting, timely authorisation, and effective behaviour support planning are critical. This article explains what restrictive practices reporting involves, when reporting is required, and how providers can stay compliant while working to reduce and eliminate these practices.
What Are Restrictive Practices Under the NDIS?
A restrictive practice is any practice or intervention that has the effect of restricting the rights or freedom of movement of a person with disability.
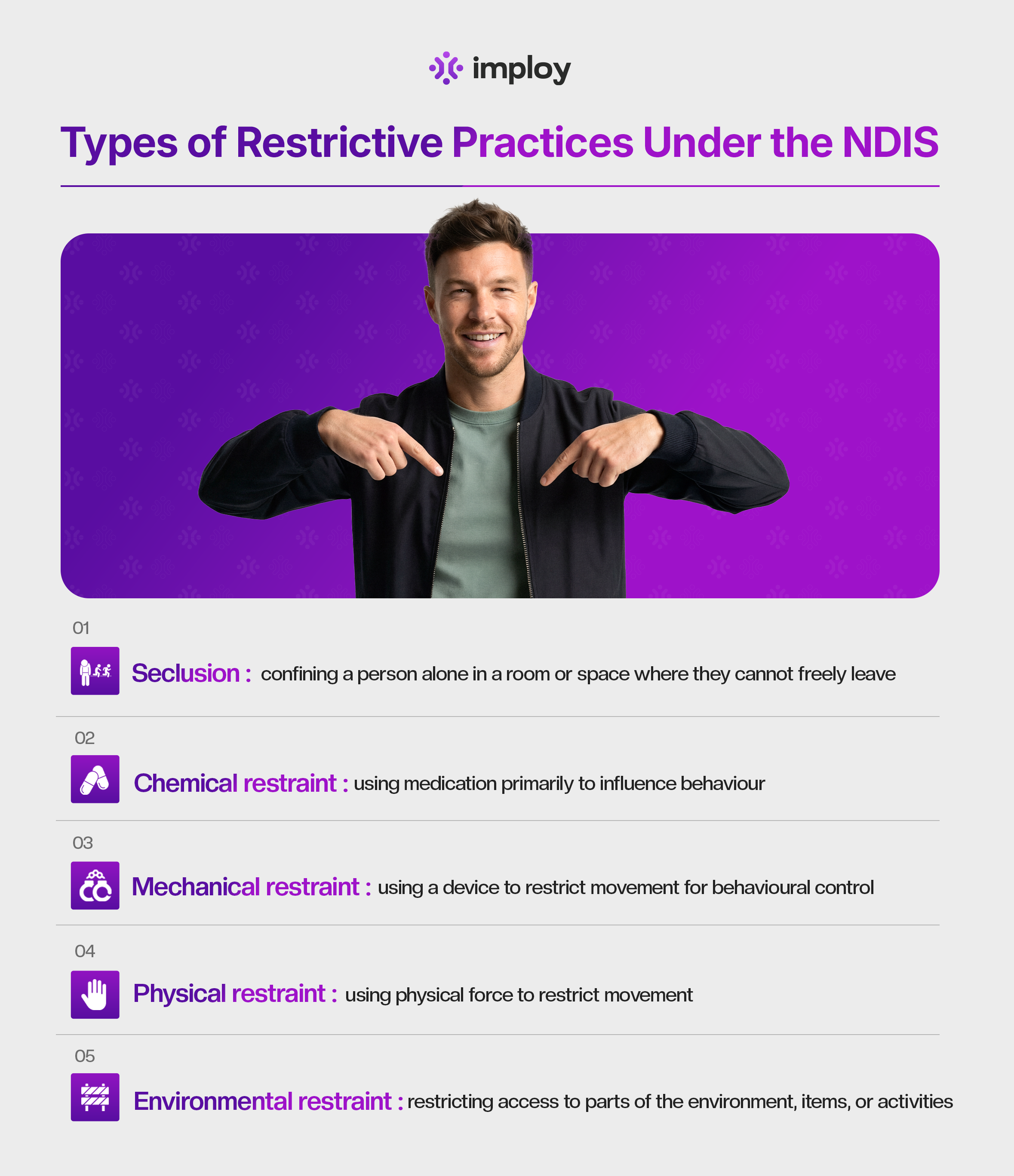
Under the NDIS (Restrictive Practices and Behaviour Support) Rules 2018, five types of restrictive practices are regulated:
- Seclusion
Seclusion involves confining a person alone in a room or enclosed space where they are prevented from leaving freely. This can occur at any time of day or night and may be explicit or implied. Because it significantly restricts a person’s freedom, its use is tightly regulated under the NDIS. - Chemical restraint
Chemical restraint refers to the use of medication for the primary purpose of controlling or influencing a person’s behaviour. It does not include medication prescribed to treat a diagnosed mental or physical condition. Chemical restraint is the most commonly reported restrictive practice and must be carefully monitored and reported. - Mechanical restraint
Mechanical restraint involves using a device to restrict a person’s movement to control behaviour. This does not include equipment used for therapeutic or safety purposes, such as mobility aids. Any behavioural use of mechanical restraint is considered a regulated restrictive practice. - Physical restraint
Physical restraint is the use of physical force to prevent or limit a person’s movement. It does not include brief, reflexive actions used to guide someone away from immediate danger. Due to the risk of physical and psychological harm, its use is subject to strict reporting requirements. - Environmental restraint
Environmental restraint restricts a person’s access to their surroundings, items, or activities. Examples include locking doors or limiting access to certain rooms or objects. While sometimes overlooked, environmental restraints are regulated and must be reported when used for behavioural control.
These practices are only regulated when they are used by NDIS providers in relation to NDIS participants. The NDIS Commission does not regulate restrictive practices used by family members, informal supports, or in settings such as health or education - unless an NDIS provider is responsible for their use in that context.
When Is a Restrictive Practice Considered Unauthorised?
A restrictive practice is considered unauthorised when:
- It has not been authorised under relevant state or territory requirements (where authorisation is required), and/or
- It is not included in a current Behaviour Support Plan (BSP) for the participant, or
- The BSP or authorisation has expired or is no longer valid, or
- A new or changed restrictive practice is used that is not covered by existing approvals.
Importantly, every individual use of an unauthorised restrictive practice must be reported to the NDIS Commission until proper authorisation is in place and a BSP has been lodged and accepted.
When Are Restrictive Practices Permitted?
It’s important to note that the NDIS Quality and Safeguards Commission does not approve or authorise restrictive practices. Instead, providers must follow the authorisation processes set out in the relevant state or territory legislation.
Restrictive practices may only be used under strict conditions. For a restrictive practice to be permitted, all of the following criteria must be met:
- The practice is clearly documented in the participant’s Behaviour Support Plan.
- Authorisation has been obtained in line with state or territory legislative requirements.
- The practice is used only as a last resort to prevent harm, after evidence-based, person-centred and proactive strategies have been explored and applied.
- The option chosen is the least restrictive response available in the circumstances.
- The practice is intended to reduce the risk of harm to the participant or others.
- The level of restriction is proportionate to the potential risk or consequences.
- The practice is applied for the shortest possible time necessary.
These principles align with Australia’s obligations under the Convention on the Rights of Persons with Disabilities (CRPD) and reflect a strong rights-based approach to disability support.
Reporting NDIS Restrictive Practices
As an NDIS provider, ensuring the safe and lawful use of restrictive practices is a critical responsibility. Any misuse or unauthorized use must be reported promptly to protect participants and meet regulatory requirements.
1. Identify Restrictive Practices
Restrictive practices include:
- Physical restraint - pinning, holding, or forcing a participant
- Chemical restraint - use of medication to control behavior
- Seclusion - isolating a participant against their will
- Mechanical restraint - using devices to restrict movement
- Environmental restraint - locking doors or restricting movement
Only practices authorized under a Positive Behavior Support (PBS) plan should be used. Any unauthorized use is reportable.
2. Follow Internal Reporting Procedures
- Immediate Action:
- Ensure the participant’s safety first.
- Remove or stop the restrictive practice if safe to do so.
- Document the Incident:
Include:
- Participant details (name, NDIS number)
- Type of restrictive practice used
- Date, time, and location
- Staff involved
- Context or behavior that triggered the practice
- Notify Internal Management:
- Report to your supervisor, manager, or internal NDIS Quality & Safeguards team.
- Follow your organization’s Restrictive Practices Policy and incident management system.
3. Report to the NDIS Commission
All providers must notify the NDIS Quality and Safeguards Commission if:
- A restrictive practice is used without authorization, or
- There is an incident or complaint relating to restrictive practices.
How to report:
- Phone: 1800 035 544 (toll-free)
- Online: NDIS Commission - Complaints & Reports
- Email: contactcentre@ndiscommission.gov.au
Information to include:
- Participant details (if available)
- Type of restrictive practice
- Description of the incident
- Staff involved
- Any supporting evidence or documentation
4. Cooperate With Investigation
- Providers are required to assist the NDIS Commission in investigations.
- This includes providing records, incident reports, and staff statements.
5. Review and Prevent
- After reporting, review policies and staff training to prevent future incidents.
- Ensure all restrictive practices used are:
- Lawful
- Authorized via a PBS plan
- Reviewed regularly for effectiveness and safety
Key Reminder:Failing to report misuse of restrictive practices can lead to regulatory action, including fines, sanctions, or suspension of your NDIS provider registration.
Reporting Pathways: How Restrictive Practices Are Regulated?
The NDIS Quality and Safeguards Commission oversees restrictive practices through two linked reporting pathways. Which pathway applies depends on whether the restrictive practice is authorised and planned, or unplanned and unauthorised.
1. Behaviour Support Reporting
Behaviour support reporting applies when a restrictive practice is approved and managed as part of a structured plan.
This pathway is used when:
- The restrictive practice has been authorised under state or territory requirements (where authorisation is required), and
- The practice is clearly documented in the participant’s Behaviour Support Plan (BSP), developed by a specialist behaviour support provider.
In these situations, the provider must:
- Lodge the BSP and any required evidence of authorisation with the NDIS Commission.
- Submit monthly reports detailing how often the restrictive practice was used, how long it was applied, and whether it aligns with the approved plan.
This reporting pathway allows the Commission to monitor the ongoing use of restrictive practices while ensuring they are being actively reviewed, reduced, and managed within a positive behaviour support framework.
2. Reportable Incidents Reporting
Reportable incidents reporting applies when a restrictive practice is unplanned, unauthorised, or used in an emergency.
This pathway must be used when:
- A restrictive practice is used as a single, emergency response to prevent immediate harm, or
- A restrictive practice is being used on an ongoing basis without authorisation or without a current BSP in place.
In these cases:
- Every individual use of the restrictive practice must be reported to the NDIS Commission as a reportable incident.
- Reporting continues until the restrictive practice is authorised (if required) and included in an approved BSP.
This pathway ensures the Commission has immediate oversight of higher-risk situations and enables early intervention to support providers in putting appropriate behaviour support plans and authorisation processes in place.
Prohibited Restrictive Practices
Some restrictive practices are never permitted due to the significant risk they pose to participant safety and wellbeing. Providers must not use the following practices under any circumstances:
- High-risk physical restraints, including:
- Forcing a participant into a face-down (prone) position.
- Forcing a participant into a face-up (supine) position.
- Pinning a participant to the ground or another surface.
- “Basket holding” or wrapping arms around a participant’s upper or lower body.
- Takedown techniques that deliberately force a participant to the floor.
- Any form of physical restraint that restricts breathing or affects digestive function.
- Forcing a participant’s head forward onto their chest.
- Applying pain, excessive force, joint hyperextension, or pressure to the chest or joints.
- Punitive or neglectful practices, including:
- Using restrictive practices as a form of punishment.
- Withholding or removing basic needs or essential supports.
These practices are strictly prohibited because they present an unacceptable risk of serious injury, trauma, or death and are inconsistent with the NDIS principles of safety, dignity, and human rights.
Key Trends in Restrictive Practices Reporting
National data shows that:
- Chemical and environmental restraints account for the majority of reported restrictive practices.
- A small proportion of participants experience a high number of ongoing restrictive practices.
- A small number of providers account for a significant share of reported incidents.
These trends have shaped the Commission’s compliance focus, with increased scrutiny on providers supporting participants with high levels of restrictive practice use and delays in behaviour support planning.
Best Practices for Managing Restrictive Practices Reporting
Leading providers embed restrictive practices reporting into everyday operations by:
- Integrating reporting with incident and risk management systems.
- Keeping behaviour support documentation current and accessible.
- Tracking authorisation and BSP expiry dates.
- Training staff to recognise restrictive practices and emergency use scenarios.
- Regularly reviewing data to identify opportunities to reduce restrictive practices.
Strong systems and clear processes are key to maintaining compliance while improving participant outcomes.
How Imploy Supports Restrictive Practices Reporting?
Imploy helps NDIS providers manage restrictive practices reporting by supporting:
- Centralised documentation of incidents and compliance records.
- Clear visibility of reporting status, follow-ups, and required actions.
- Consistent record-keeping aligned with audit and compliance expectations.
- Better oversight across participants, incidents, and risk areas.
By streamlining compliance processes, Imploy supports providers to focus on safe, rights-based service delivery.
Final Thoughts
Restrictive practices reporting is not just a regulatory requirement - it is a critical safeguard designed to protect participants and promote positive behaviour support.
For NDIS providers, staying compliant means understanding when reporting is required, acting quickly to obtain authorisation and behaviour support plans, and maintaining strong systems to monitor and review practice over time.
With the right processes, training, and tools in place, providers can meet their obligations while actively working toward the reduction and elimination of restrictive practices - the ultimate goal of the NDIS framework.
Frequently Asked Questions (FAQs)
1. Do all restrictive practices need to be reported?
Yes. Every use of a restrictive practice must be reported to the NDIS Quality and Safeguards Commission. If the practice is authorised and included in a current Behaviour Support Plan (BSP), it is reported through monthly behaviour support reporting. If it is unauthorised or used as a single emergency response, it must be reported as a reportable incident.
2. What happens if a Behaviour Support Plan or authorisation expires?
If a BSP or authorisation expires, any continued use of a restrictive practice becomes unauthorised. Each instance must then be reported as a reportable incident until a new BSP is lodged and authorisation is reinstated.
3. Are medications always considered chemical restraint?
No. Medication is only considered a chemical restraint if it is used primarily to influence behaviour. Medication prescribed to treat a diagnosed mental health condition, physical illness, or medical condition is not considered chemical restraint under the NDIS.
4. Do restrictive practices used by families or informal supports need to be reported?
No. The NDIS Commission only regulates restrictive practices used by NDIS providers. Practices used by family members or informal supports are not reportable unless an NDIS provider is responsible for their use.
5. What happens if a provider fails to report restrictive practices?
Failure to report can lead to compliance action, including investigations, conditions on registration, or enforcement measures. It can also impact audit outcomes and place participants at risk.