How to Create an NDIS Incident Report (Step by Step for Providers)
NDIS incident reporting made simple: A step-by-step guide for providers to document, track, and resolve incidents efficiently with imploy.
If you’re an NDIS provider, you already know that things don’t always go to plan. Participants may have accidents, unexpected events can occur, or serious situations might arise that put people at risk. When they do, you have a responsibility to respond, and part of that responsibility is completing an NDIS incident report.
But here’s the good news: incident reporting doesn’t have to be overwhelming or stressful. Think of it as a way to protect participants, support your team, and make your service stronger. In this guide, we’ll walk you through how to create an NDIS incident report step by step, so you can feel confident about doing it right every time.
What exactly is an NDIS Incident?
The NDIS Quality and Safeguards Commission defines an incident as ‘any event that has caused harm, or could have caused harm, to an NDIS participant while receiving services or support.’
The NDIS incident reporting process is there to make sure that when something serious happens, it’s properly recorded, managed, and resolved. It follows the NDIS guidelines to protect the safety and wellbeing of participants, while also helping providers meet their legal and regulatory responsibilities.
Some examples include:
- A participant being seriously injured.
- Allegations of abuse, neglect, or exploitation.
- Sexual misconduct.
- A participant going missing.
- The death of a participant.
There are two main types:
- Reportable incidents: these must be notified to the NDIS Commission within strict timeframes.
- Non-reportable incidents: not always reported to the Commission but still recorded internally for safety and compliance.
Why Does Reporting Matters?
Reporting isn’t just a box to tick for compliance, it’s about people. When done well, it creates a safer, more supportive environment for everyone involved.
- It keeps participants safe and shows them their wellbeing comes first.
- It helps staff learn and respond better when challenges arise.
- It reassures families and guardians that their loved ones are in good hands.
- It protects your organisation from risks and penalties.
- Most importantly, it builds trust with the people who rely on your care every day.
In many ways, incident reporting is like a safety net - catching problems early, protecting participants, and giving providers the chance to improve.
What’s Considered a Reportable Incident?
Not every incident needs to be reported to the NDIS Commission, but some serious events do. These are called reportable incidents, and they must be reported within strict timeframes because they have a big impact on a participant’s health, safety, or wellbeing.
Here are the main types:
- Death: If a participant passes away while receiving NDIS services, it must always be reported, no matter the cause.
- Serious injury: Injuries that need medical treatment or hospitalisation, such as broken bones, deep cuts, or head injuries.
- Abuse or neglect: This can be physical, emotional, psychological, or financial abuse, as well as failing to provide proper care.
- Unlawful physical or sexual contact: Any kind of assault, inappropriate behaviour, or non-consensual contact with a participant.
- Sexual misconduct: Inappropriate sexual behaviour such as harassment, grooming, or exploitation.
- Unauthorised restrictive practices: Using restraints or seclusion without the correct consent or authorisation.
These rules may feel strict, but they’re designed for one reason: to protect participants and make sure they always feel safe, supported, and respected.
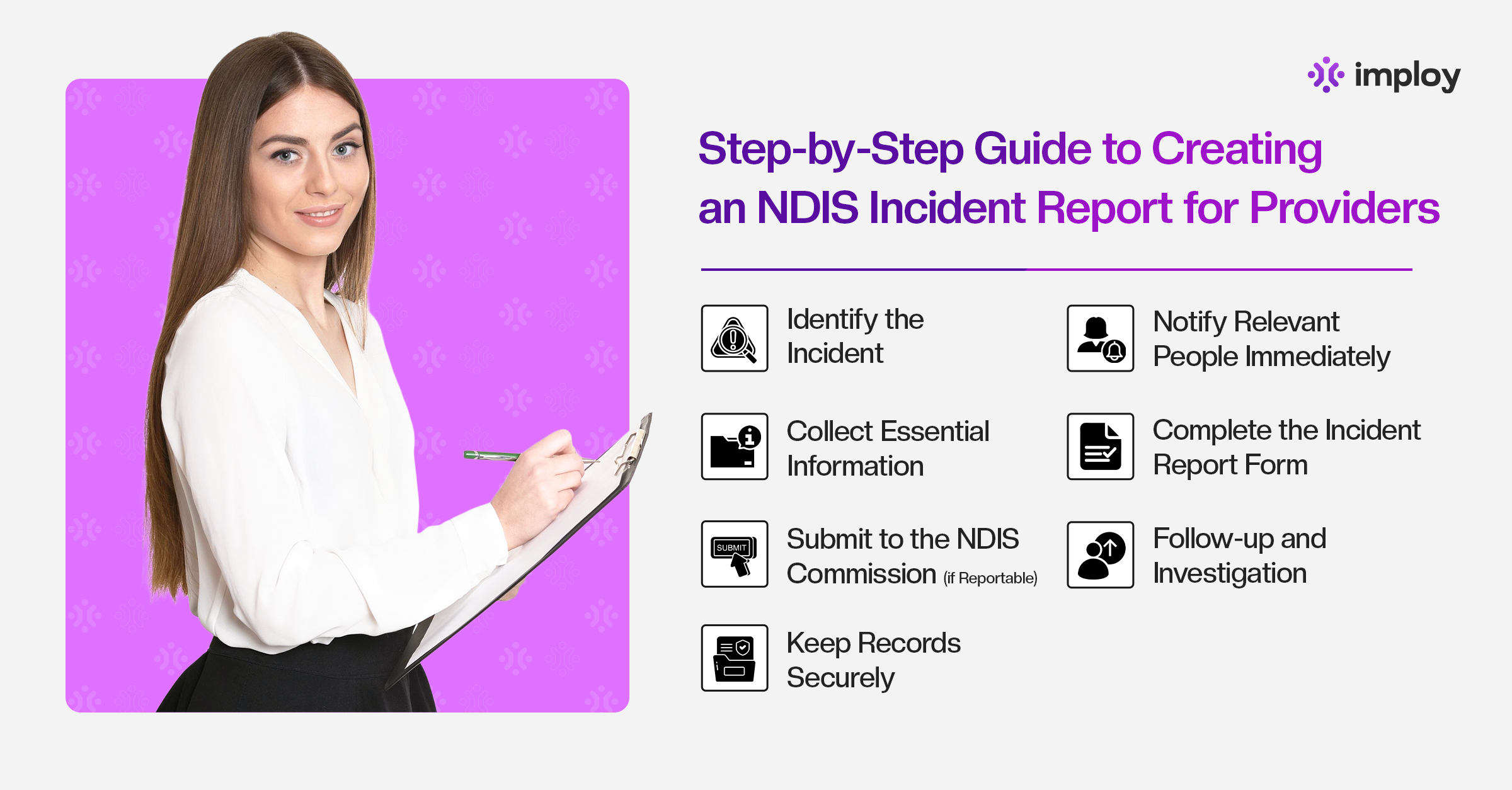
Step-by-Step: How to Create an NDIS Incident Report
The NDIS incident reporting process is there to make sure that when something serious happens, it’s properly recorded, managed, and resolved. It follows the NDIS guidelines to protect the safety and wellbeing of participants, while also helping providers meet their legal and regulatory responsibilities.
Here’s a practical breakdown of what to do when something happens:
Step 1: Identify the Incident
An incident is any event that puts an NDIS participant’s health, safety, or wellbeing at risk. This might be something obvious, like a fall that causes an injury or an accident requiring medical attention. But it also includes less visible harms, such as emotional distress, neglect, or psychological abuse.
In short, if something happens that could cause a participant to feel unsafe, disrespected, or harmed, whether physically or emotionally, it should be treated as an incident. Recognising and reporting these moments quickly is the first step in making sure participants are protected and supported, while also helping providers prevent similar issues in the future.
Step 2: Notify Relevant People Immediately
Once the situation is safe, the next step is to notify the right people. This usually includes your manager or designated incident officer, and in serious situations, emergency services. It’s also important to inform the participant’s family, guardian, or support coordinator where appropriate.
For reportable incidents, such as death, serious injury, abuse, neglect, or sexual misconduct, the NDIS Commission must be notified within 24 hours.
Step 3: Collect Essential Information
Before writing the report, gather as much detail as possible. The information may include:
- Participant details (name, NDIS number).
- Date, time, and exact location.
- Type of incident (injury, abuse, accident, missing person, etc.).
- People present or witnesses.
- Immediate actions taken.
Step 4: Complete the Incident Report Form
When filling out the report, focus on the facts. Avoid making assumptions or including personal opinions. Use clear and professional language, explain what happened, when it happened, and who was involved, and attach any supporting documents such as medical reports or staff notes. The goal is to create a clear, objective record of the event.
Step 5: Submit to the NDIS Commission (if Reportable)
If the incident is considered reportable, it must be submitted to the NDIS Commission through their online portal. Serious cases such as death, serious injury, abuse, neglect, sexual misconduct, or missing participants must be reported within 24 hours, while other reportable incidents can be lodged even after 24 hours of the incident.
Step 6: Follow-up and Investigation
After an incident is reported, the next step is to look deeper into what happened, especially if the situation was serious. This follow-up may involve collecting additional details, speaking with staff or witnesses who were present, and reviewing any records or evidence related to the incident.
In some cases, a formal investigation may be required to understand the root causes. The aim isn’t just to document what went wrong, but to identify patterns, gaps, or risks that could be addressed to prevent the same thing from happening again.
Step 7: Keep Records Securely
Finally, all incident reports should be stored securely to meet compliance and privacy requirements. Keeping accurate records also allows providers to identify patterns and use incidents as learning opportunities to improve service quality.
Best Practices for Providers
The most effective NDIS providers don’t just respond to incidents, they plan for them. Being proactive helps protect participants, support staff, and strengthen your organisation’s overall service quality. Here are some best practices to keep in mind:
- Train your staff regularly: Make sure everyone knows how to recognise incidents, respond appropriately, and report them quickly. Ongoing training builds confidence and ensures that everyone acts consistently and safely when incidents occur.
- Foster a culture of open reporting: Encourage staff to speak up without fear of blame or punishment. When your team feels safe to report mistakes, near-misses, or concerns, it helps catch potential risks early and prevents more serious incidents down the line.
- Review and learn from incidents: Don’t let reports sit in a folder. Regularly analyse incident data to identify patterns, trends, and areas for improvement. Use these insights to refine policies, update procedures, and provide targeted staff training.
- Leverage digital tools like imploy: Modern software makes incident reporting faster, easier, and more reliable. imploy provides structured forms, automated alerts, secure record storage, and audit-ready reports, helping your team focus on participant care rather than paperwork.
By embedding these practices into daily operations, providers create a safer, more responsive, and accountable environment - ultimately improving the experience and wellbeing of participants.
How imploy makes Incident Management Easier?
Here are several ways imploy helps providers manage incidents more effectively. These aren’t just features - they’re tools that reduce risk, save time, and ensure compliance.
1. Structured Incident & Risk Logs
imploy offers a comprehensive incident log where staff can easily submit, track, and resolve incidents, giving full visibility from the moment an incident is reported. Supporting evidence, such as photos or documents, can be uploaded directly into the record, so there’s no need to chase paperwork later.
The platform also includes follow-up and resolution tracking, allowing providers to document actions taken to address the incident, whether that’s medical treatment, policy updates, or staff retraining and see clearly when each incident is fully resolved.
2. Compliant Templates
To make incident reporting easier and more reliable, imploy provides ready-made templates that are fully compliant with NDIS standards. This means providers don’t have to create their own forms or worry about missing essential fields.
The templates also help ensure consistency across the team, which is especially important when multiple staff members are submitting reports, as it reduces the risk of errors or overlooked information.
3. Real-Time Activity Logs and Digital Trails
Every action recorded in imploy is timestamped and version-controlled, providing a clear record of who did what and when. This creates a transparent digital trail that supports accountability and makes audits much easier.
Additionally, any delays in follow-up or missed steps, such as missing signatures or late updates are easy to spot, helping providers reduce the risk of non-compliance and maintain high standards of care.
4. Compliance Alerts & Document Tracking
imploy also helps providers stay on top of compliance by sending automated expiry notifications for staff certifications, care plans, service agreements, and more, ensuring that no required document lapses unnoticed. Its document compliance dashboards provide a clear overview of what’s current and what requires attention, reducing surprises and making it easier to respond confidently during audits.
5. Customisable & Exportable Reports
imploy allows providers to create custom reports filtered by criteria such as funding type, service type, staff member, region, or client, giving the flexibility to track incident trends or compare data across the organisation.
Reports and summaries can be easily exported in PDF or CSV format, making them convenient to share with stakeholders, auditors, or for internal review meetings. Additionally, report templates can be saved for recurring reporting needs, so you don’t have to start from scratch each time, streamlining the process and ensuring consistency.
Use our incident report template to help you create your own incident report document.
Final Thoughts
Incident reporting is an essential part of providing safe, high-quality NDIS services. While it might feel overwhelming at first, following a structured process ensures that participants are protected, staff are supported, and your organisation stays compliant.
By recognising incidents quickly, documenting them accurately, and following up appropriately, providers can turn every incident into a learning opportunity that improves service delivery. Tools like imploy make this process faster, more reliable, and audit-ready, giving your team more time to focus on what truly matters i.e participant care.
Frequently Asked Questions (FAQs)
1. What is the difference between a reportable and non-reportable incident?
Reportable incidents are serious events that must be notified to the NDIS Commission within strict timeframes, such as death, serious injury, abuse, or sexual misconduct. Non-reportable incidents still need to be recorded internally but do not require submission to the Commission.
2. How quickly do I need to report a serious incident to the NDIS Commission?
Serious incidents, including death, abuse, neglect, sexual misconduct, or serious injury, must be reported within 24 hours of becoming aware of the incident.
3. Can minor incidents be ignored?
No. Even minor incidents should be documented internally. Recording all incidents helps identify patterns, prevent future risks, and supports continuous improvement in care.
4. What information should I include in an incident report?
Key details include participant information, date, time, and location of the incident, type of incident, people involved or witnesses, and the immediate actions taken. Any supporting evidence, such as photos or medical reports, should also be attached.
5. How does using software like imploy help with incident reporting?
Imploy streamlines the process by offering structured incident logs, compliant templates, real-time activity tracking, compliance alerts, and customisable reports. This reduces paperwork, ensures audit readiness, and allows your team to focus more on participant care.