How to Write Nursing Progress Notes: A Practical Guide
Explore the key elements of nursing progress notes and how they enhance patient care and communication among healthcare teams.

Accurate nursing notes are key in maintaining continuity of care. According to the Department of Health, Disability and Ageing, there are over 350,000 individuals registered with the Nursing and Midwifery Board of Australia as of 2025. These professionals are an interconnected network within the healthcare industry that work in tandem at every level with varying levels of experience, different backgrounds, areas of expertise and capabilities. Moreover, as part of their formal education, these professionals are trained to craft progress notes in the clinical setting. The notes serve as legal documentation, enhance communication among healthcare professionals and support client safety. Given their significance, here are tips for nursing professionals to also master the art of writing effective and accurate progress notes for clients participating in the National Disability Insurance Scheme (NDIS), Home Care Packages (HCP) program, and Commonwealth Home Support Program (CHSP).
The staples of a progress note are,
Date and Time: Record of the exact time and date when care was provided or situation observed
Client Information: The client’s name and identifying information
These details are recorded without fail after every encounter with the client. Additionally, there are only a few accepted formats used to record and relay essential information on the clients’ condition:
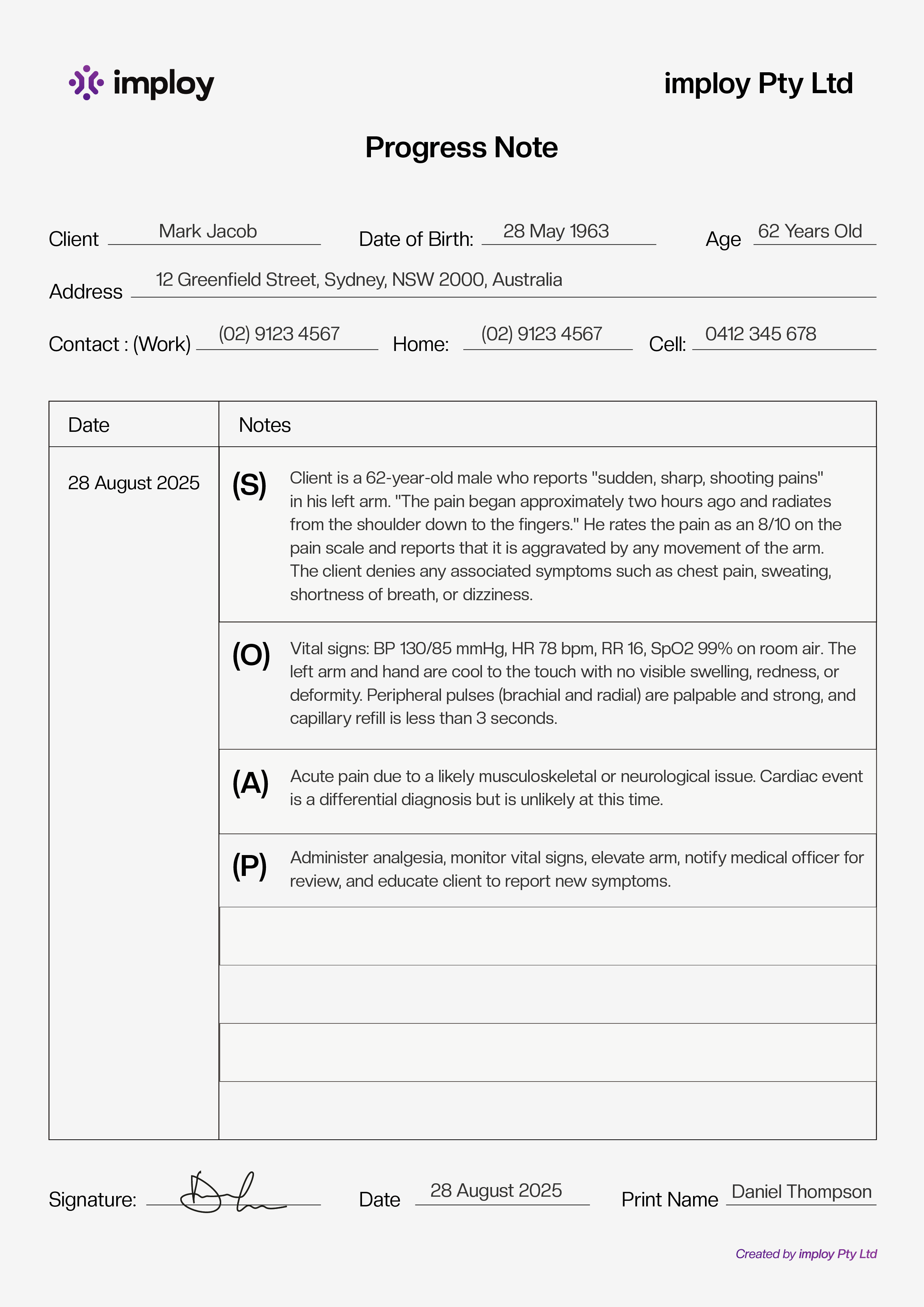
SOAP (Subjective, Objective, Assessment, Plan): The SOAP format is ideal for an initial assessment and comprehensive visits. The subjective (S) notes the nature of the client’s ailments. Use direct quotes on pain, effect of medication, and current feeling. The objective (O) is a record of the client’s weight, blood pressure, temperature, lab results (if any), and physical exam findings. An assessment (A) is the nurse’s diagnosis. It is structured as a statement on why a client might be experiencing symptoms. The Plan (P) outlines the next step in addressing the subjective. The SOAP format is compliant with clinical documentation standards globally.Written in the SOAP format, there are a few key phrases used to describe a client’s case to the NDIA. For best practice, you can also refer to Imploy’s NDIS progress notes template, which is tailored to align with NDIA requirements.
DAR (Data, Action, Response): The DAR format is similar to SOAP, however, nurse’s entries focus on an incident in the clinical setting. The Data (D) summarizes the client’s problem relative to the incident and evidence to corroborate the claim. The Action (A) notes the nurse’s activity to address the client’s condition. The entry can be as succinct as “Spoke to [Client’s Name] calmly”. The Response (R) records the client’s condition after action to communicate the incident’s severity to the involved professionals administering care.
PIE (Problem, Intervention, Evaluation): The PIE format is designed to track the progress of a treatment plan for a client. The Problem (P) is written in the form of a nursing diagnosis. The Intervention (I) outlines an action or a necessary step in the treatment plan. The Evaluation (E) records the results of intervention. Deviation from the plan to address unexpected problems is common in healthcare and the PIE format is designed to document this volatility. Nurse’s entries can advise deviations in the treatment plan based on the severity of the problem and the extent of the intervention.
These structured documentation formats are the norm in the healthcare industry for clarity among the care team. Avoid deviation from these formats—use Imploy Healthcare’s ready-to-use NDIS progress notes template to simplify compliance, or download a free support worker progress notes template for everyday care documentation.
There is an added caveat to writing progress notes for participants in the National Disability Insurance Scheme (NDIS). A client is considered to be eligible for NDIS if they have “lifelong and substantially reduced functional capacity” that impairs their ability to manage themselves. Thus, the language of diagnosis or treatment isn’t necessarily applicable in progress notes that the National Disability Insurance Agency (NDIA) monitors to assess a client’s eligibility for government assistance. Written in the SOAP format, there are a few key phrases used to describe a client’s case to the NDIA.
Functional impact: The impact of a condition on the broad domains of a person’s life. A concise entry in the progress note describing how the client’s condition affects their neurological state often written with direct quotes. Add the client’s cognitive and intellectual abilities in relation to the people around them, and their sensory, physical, or psychiatric function.
Functional capacity: Professional assessment of how much help a client might need in completing important everyday activities, and fulfilling social and economic roles.
Functional impairment: Impairment is a recognised intellectual, cognitive, neurological, sensory, physical or psychiatric condition identified by a qualified professional as affecting a person. The language used in describing the impairment is a statement on the abnormal state of a client’s health, thus it should describe problems the client has in accomplishing everyday activities.

Kir Larwill, Gill Hilton and Cathy Bucolo, in their text “Getting the Language Right”, recommend crafting progress notes as a record of “building capacity” in the client to maintain an independent and dignified life around their functional impairment. Instead of “simply assisting them with tasks”, the care provider crafting these notes for the care team can resourcefully share a care plan using the PIE format to build the client’s confidence in doing tasks for themselves.
Carefully constructed progress notes build core activities for the client. New and existing support workers benefit from clearly written reports and the client receives continued care. These tasks are key in fulfilling the major criteria for receiving aid from the NDIS – the participant’s rehabilitation. A glossary for key terms from the NDIS is available here. Modern healthcare software like Imploy have AI enhanced insights for nursing progress notes. Refining entries to fit NDIA’s criteria is crucial is securing funding for care. With these additional features, even support workers without formal training in progress report writing receive summaries on existing entries for seamless communication between the extended care team.
Similarly, the HCP and CHSP’s goal is to assist older adults to live independently. Nursing progress notes in the DAR format are indicators for the client’s health and condition. Data on their well-being is crucial to medical professionals as well as their families.
Older adults may need additions at their residence to ensure their safety and promote independence. To secure capital for home improvement, the care provider’s progress note must address their client’s functional capacity effectively to justify spending allotted funds on any project. Therefore, the language used in reports incorporates quotes from the clients stating recurring issues and offers a professional recommendation on the extent of intervention required for rehabilitation.
The language used in drafting said recommendations to the governing body must clearly position the installation of additional support in the client’s home as “capacity building”. Support that enables the client to build an independent lifestyle. Positioning home improvement projects as core support to enable the client to complete daily activities ensures there are no disputes with deploying the funds. Describe how the client’s care arrangements account for the change in their lifestyle due to their condition. Write a detailed description of the proposed home modification project. Add why the client can no longer continue functioning independently with existing infrastructure. Refrain from giving opinions and vague recommendations.
A participant in the NDIS, HCP, and CHSP has formal and informal care providers. Informal support can come from anybody in their vicinity. Thus, for legibility in any draft of a progress note, avoid repetition in between sections, use the client’s own words where applicable, and use the right language that leads to the desired outcome for the client. Vague description often leads to miscommunication. Take the word “stable” for example. In clinical research, the word “stable” refers to conditions that are neither regressing nor progressing in the client. Whereas, in a medical setting, using the word “stable” refers to the normal condition of the client’s vital signs. Avoid nuances in language and add a sentence that offers clarity. Tools for healthcare providers, like Imploy’s AI summary feature will provide concise recommendations if the entry is specific and detailed.
FAQ
Q1: Why are nursing progress notes important in NDIS, HCP, and CHSP care?
A: Accurate progress notes ensure continuity of care, improve communication among care teams, serve as legal documentation, and help secure funding for client support. For NDIS participants, detailed notes are essential to demonstrate functional impact, capacity, and impairment for NDIA reviews.
Q2: What are the key elements of a progress note?
A: Every progress note should include:
- Date and Time: Record when care was provided or the observation occurred.
- Client Information: Name and identifying details.
- Structured Format: Use accepted formats such as SOAP, DAR, or PIE for clarity and compliance.
Q3: What is the SOAP format and when is it used?
A: SOAP (Subjective, Objective, Assessment, Plan) is ideal for initial assessments and comprehensive visits:
- S (Subjective): Client-reported symptoms and quotes.
- O (Objective): Measurable data such as vitals or lab results.
- A (Assessment): Nurse’s professional evaluation or diagnosis.
- P (Plan): Next steps for care or intervention.
Imploy Healthcare provides NDIS-tailored SOAP templates aligned with NDIA requirements.
Q4: What is the DAR format?
A: DAR (Data, Action, Response) focuses on incidents:
- D (Data): Summary of the problem or incident.
- A (Action): Steps taken to address it.
- R (Response): Client’s outcome after intervention.
This format is particularly useful in HCP and CHSP settings for documenting daily care events.
Q5: How does the PIE format work?
A: PIE (Problem, Intervention, Evaluation) tracks treatment progress:
- P (Problem): Nursing diagnosis.
- I (Intervention): Action taken to address the problem.
- E (Evaluation): Outcome or effectiveness of the intervention.
This format allows documentation of deviations and helps in rehabilitation-focused care.
Q6: What special considerations apply to NDIS progress notes?
A: NDIS participants must be documented based on:
- Functional Impact: How the condition affects daily life and independence.
- Functional Capacity: Assessment of assistance required.
- Functional Impairment: Intellectual, cognitive, sensory, or physical limitations.
Language should focus on “capacity building” rather than just completing tasks for the client.
Q7: How do progress notes support funding and home modifications?
A: Clear documentation justifies NDIS or HCP funding for care or home adaptations. Notes must explain:
- Why the client cannot maintain independence with existing infrastructure.
- How proposed interventions build the client’s capacity.
- Professional recommendations backed by client quotes and observations.
Q8: How can Imploy Healthcare help with progress notes?
A: Imploy Healthcare offers:
- Ready-to-use NDIS progress note templates in SOAP, DAR, and PIE formats.
- AI-enhanced summaries to refine notes for NDIA criteria.
- Consistency across support workers, ensuring clear communication and compliance.


.jpeg)